RESEARCH BRIEFING – WEEK IN REVIEW
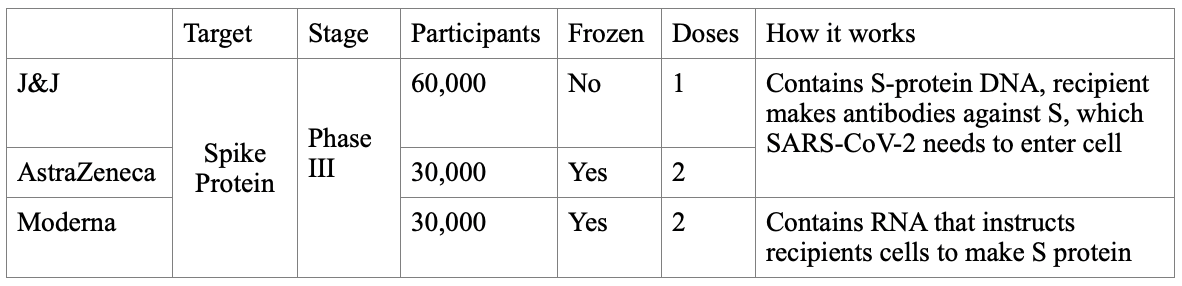
Johnson & Johnson released a study protocol last week, describing a plan to enroll 60,000 patients across the United States for its phase III trial designed to assess the safety and effectiveness of its candidate for a SARS-CoV-2 vaccine. In this brief we compare the Johnson & Johnson, AstraZeneca and Moderna vaccines. All three companies have candidate vaccines in Phase III trials that target the S protein.
These vaccines share a common strategy of prompting the body to generate antibodies that recognize SARS-CoV-2 virus particles, surround the particles and mark them for destruction. Johnson & Johnson and AstraZeneca have used a more traditional approach. These two are created by splicing DNA for the S-protein of SARS-CoV-2 into the genome of a carrier virus. This carrier virus can infect human cells but it cannot replicate. Johnson & Johnson uses Ad26, an adenovirus, while AstraZeneca uses ChAdOx1, a chimpanzee adenovirus. The Moderna vaccine uses nanoparticles to deliver RNA encoding the S-protein. The table above summarizes the three vaccines.
The high-level view is that targeting the S-protein is likely to provide immunity against this version of SARS-CoV-2. New vaccines may be required each year and the vaccine may be more effective in some years than others. Furthermore, some vaccine approaches may be more effective in certain groups. For example, the Moderna vaccine may be safer in patients with autoimmune conditions, because it does not use a functioning virus. One barrier that each of these candidates carry a logistical component to their success, as they all require some degree of refrigeration, which will complicate delivery and storage to areas with less infrastructure. 28 September 2020.
SARS-CoV-2 causes illness directly by infecting cells and indirectly by provoking an infected person's body to retaliate in a self-destructive manner. In particular, SARS-CoV-2 is thought to increase the risk of blood clots in the lungs, which can itself be life-threatening, as such clots block the flow of blood in the lungs and therefore prevent the delivery of oxygen into the bloodstream and to the rest of the body. This combination of direct and indirect harm is not unique to SARS-CoV-2, or even the coronavirus family. Infections can cause prolonged pain (herpes viruses), bone marrow failure (parvoviruses) and are linked to cervical cancer (human papillomaviruses) and lymphoma (Epstein-Barr viruses). In addition, many different viral and bacterial infections are linked to myocarditis, a life-threatening infection of the heart, while others can cause the thyroid to go through dangerous periods of overactivity or underactivity.
A recent study in The Lancet aimed to better understand the biology behind this increased risk by performing detailed autopsies on 21 patients, aged 41-78, who died of complications from covid-19. The authors found overabundant inflammatory cells through the body including in the brain and blood. One type of inflammatory cell, the neutrophil, can jumpstart clotting if they are present in large numbers. The authors did not find high levels of circulating virus nor any evidence of the virus sheltering in various organs or in the inflammatory cells themselves. Even as levels of SARS-CoV-2 decreased in patients, they became gravely ill, which led the study's authors to hypothesize that the body's exuberant inflammatory response may be behind some of covid-19's mortality. This is similar to how we now think of sepsis; that condition is triggered by infections but is driven by the body's counterproductive and ultimately harmful response to them.
There are notable limitations to the Lancet study, however. First, it only involved 21 fatal cases, a relatively small number. Second, information gleaned from autopsies can be tricky, as tissue degradation between death and the time of autopsy may inadvertently decrease estimates of the viral load. Additionally, there was no comparison group to determine whether the burden of clots observed is greater when compared to death by other causes including serious viral infections other than SARS-CoV-2; it is important to realize that clots also form naturally in deceased bodies as stationary blood pools and hardens. Despite these limitations, this study is an important reminder of our incomplete understanding of SARS-CoV-2 infection and our body's responses. Until that knowledge is more complete, our most effective tool against covid-19 remains public health measures that limit our exposure, though hopefully a vaccine will be our next line of defense. 1 October 2020.
The accelerated covid-19 vaccine research has led to the release of many recent notable manuscripts and another was published this week in the New England Journal of Medicine that analyzed an important high risk group: older adults. Conducted at three sites across the United States (Kaiser Permanente research center in Seattle, Emory University and the National Institute of Allergy and Infectious Diseases NIAID) this Phase 1 vaccine study was expanded to include forty older adults. The subjects were divided into two groups, 56-70 years old and those 71 and older. Interestingly, participants were not screened for past or current covid-19 infection before enrollment.
The vaccine being tested was developed by the National Institute of Allergy and Infectious Diseases and Moderna, a biotechnology company in Cambridge, MA. It utilizes the S protein by which the coronavirus enters host cells. Participants received either 25 micrograms or 100 micrograms of the injection. Each person received an injection on day 1 and 29 with the same dose given each time. Follow-up visits were performed on days 7, 14 and 57. Following vaccination, an assessment of antibody and T-cell response was studied. The 100 microgram dose (higher) dose exhibited higher binding- and neutralizing-antibody titers compared to the 25 microgram dose.
Of the 40 patients, one in the 56-70 year lower dose group did not receive the second dose after developing a fingernail infection which required antibiotic treatment. Common side effects such as headache, fever, body aches, chills and injection site pain were reported which were all classified as mild to moderate and were often associated with the second dose.
This small Phase 1 study of older adults shows promise in a vaccine for covid-19 and appears to be effective and well tolerated in older adults. It remains early. The question of long-standing immunity and the ability of these antibodies to prevent infection remains unanswered. 2 October 2020.